Client
St Joseph's Healthcare
Overview
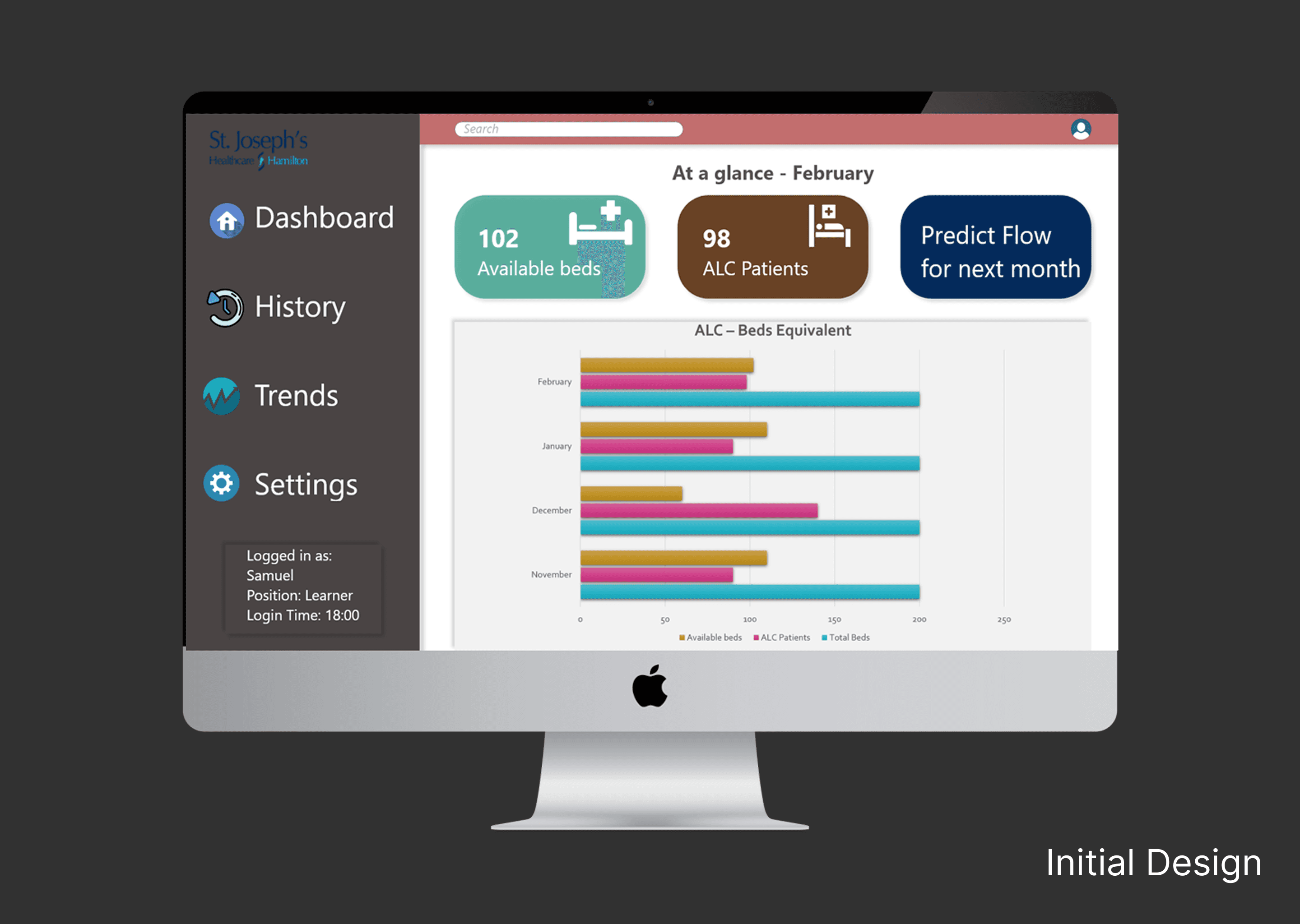
One out of six beds in the acute care setting is occupied by an Alternate Level of Care (ALC) patient, which creates a shortage of beds for patients who are in actual need of them in the hospitals. This is due to several reasons including the prolonged time that is taken during decision-making for shifting patients from acute care to other care settings. The purpose of this project was to design a decision-aid tool to improve the ALC patient experience of those in the process of being transferred to the Alternate Care Setting and subsequently to their next level of care destination.
Client
St Joseph's Healthcare
Industry
Healthcare
Service
UI / UX Design
User Research
Process Optimization
Duration
8 Months
The Problem
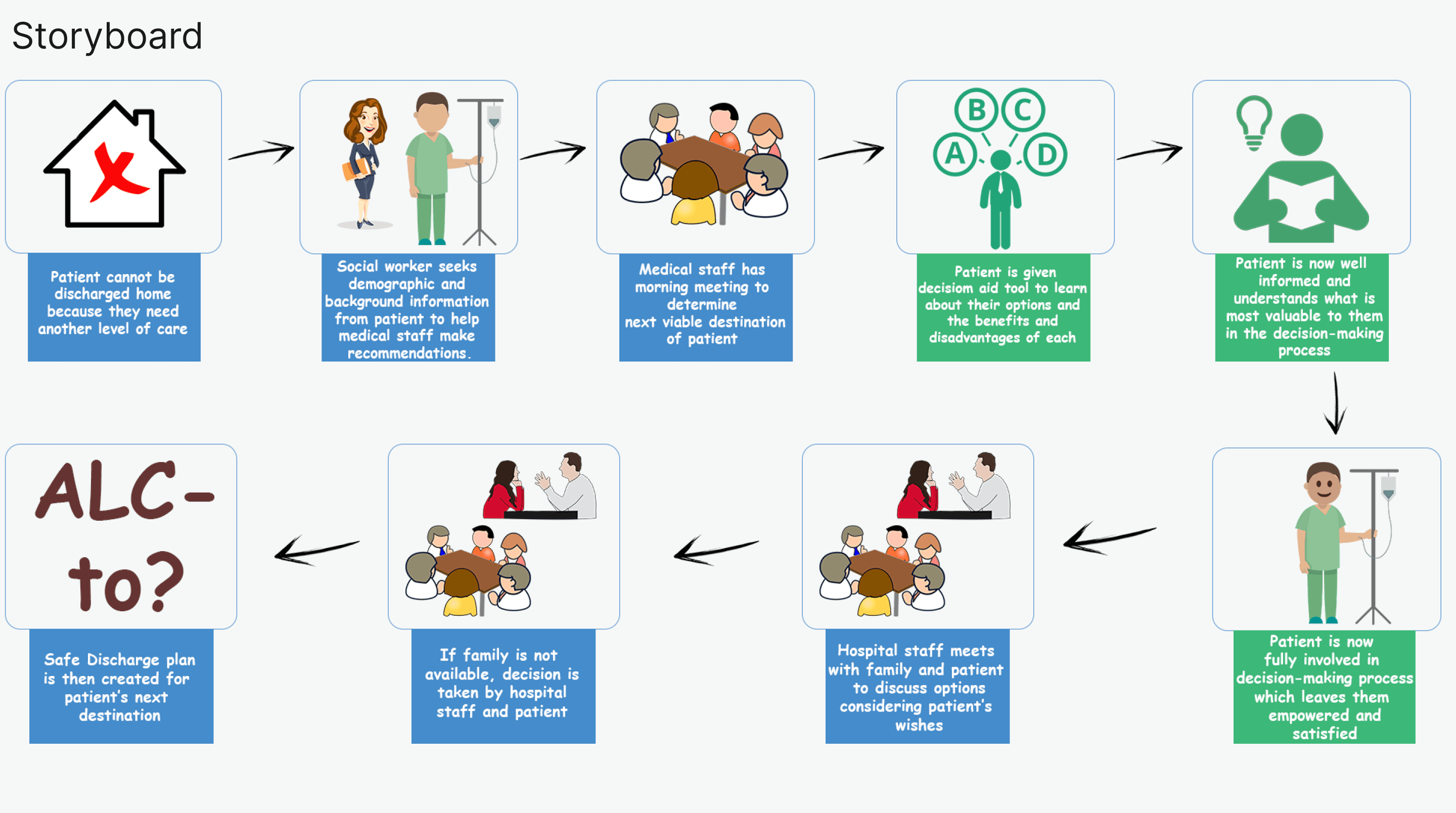
In our research prior to the inception, we realized that the recommended decisions taken about the next discharge destination of patients do not include the patient from the start. The patient is only somewhat involved at the tail end of the process. This led to patients' choices mostly not considered if it conflicted with the hospital’s recommendations, and subsequently slowed down the decision making process, which in turn led to slow processing times and unavailablity of hospital beds for incoming patients. At the project's inception, our objective was to analyze the movement of ALC (Alternative Level of Care) patients within the hospital, utilizing this data to guide decision-making and enhance patient flow. However, the arrival of the COVID-19 pandemic significantly restricted our interaction with the hospital. As designers, we confronted the challenge of adapting our approach while addressing the same underlying issue. This led us to uncover a bottleneck in the decision-making process, prompting us to explore alternative solutions.
My Approach
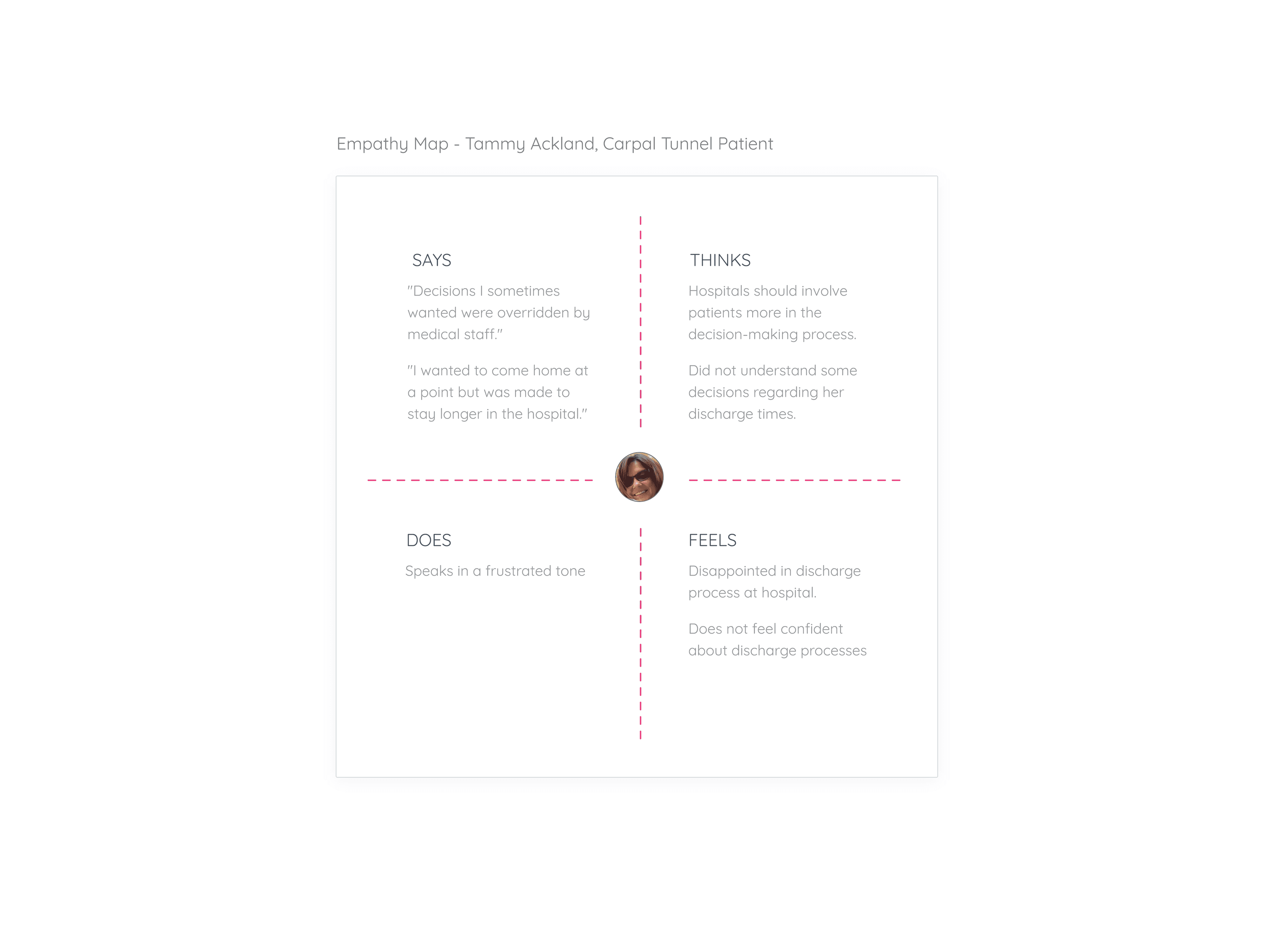
Stakeholders Interviewed - 5 (four nurses, 1 patient) User interviews were conducted to learn more about the current situation, and how things could be improved. Some of the questions that were asked included: 1. What is the current decision-making process like?What are the factors that speed up or delay ALC designations? 2. How does the patient feel when waiting? 3. Do they know how long they must wait?How can we enhance the waiting experience for the patient? 4. How do their families react to the waiting times?How do patients react when told they have been put into ALC status? 5. Is technology needed to solve this issue? 6. Why is the existing solution not working? Insights 1. Patients are usually devastated and just want to go home. 2. The family of patients usually plays a larger role in determining the ALC status. 3. The decision-making times are usually not included in the factors that lead to higher wait times but play a huge role. 4. Some patients enjoy being in the hospital, others don’t. 5. Every situation is extremely different. 6. Alc processes differ from department to department 7. Every ALC patient has a designation. 8. A safe discharge plan takes about 2 weeks. Adds to wait the time. In all of this, we were most curious to find out if any processes slowed down the overall waiting time but had not been considered much by the stakeholders, and we discovered that the decision-making process of ALC patients moving from an ALC setting to another setting was one such processes.
The Solution and Impact
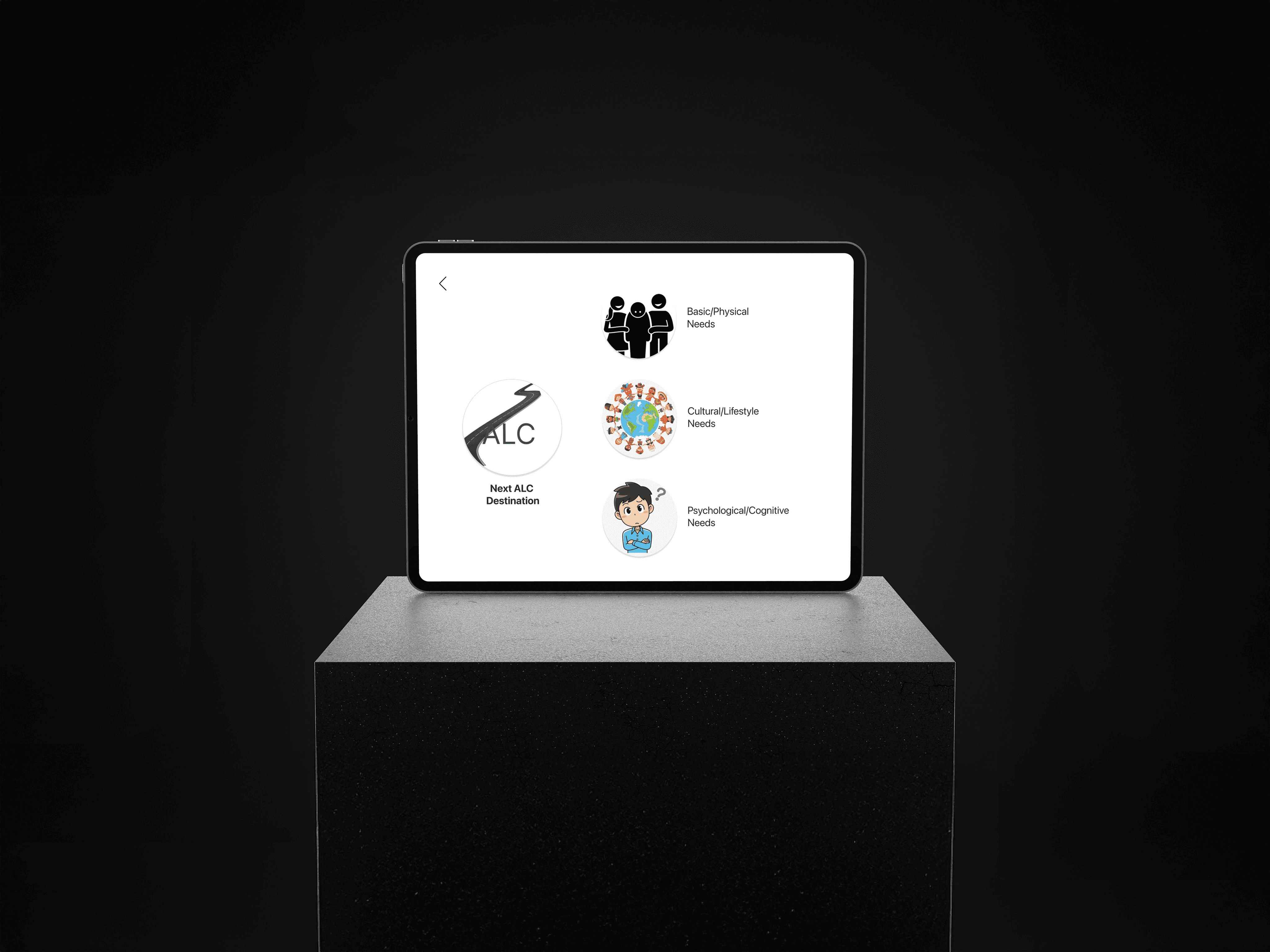
The ultimate objective of this design was to empower patients to make informed decisions about their next destination following ALC, resulting in reduced wait times and enhanced patient care experiences. By facilitating faster and more accurate decision-making, this tool contributed to the overall efficiency and seamless operation of the hospital, delivering benefits to both patients and healthcare providers. It was indeed a win-win situation for all parties involved. We used the H.E.A.R.T Framework as our KPI tool in this project. We tested with 5 users and measured these outcomes. Happiness - 4/5 Engagement - 4/5 Adoption - 3.5/5 Retention - 3.5/5 Task Success - 4.5/4